
I. Basic Cardiac Function
The human heart is made up of two mechanical pumps (right and left hearts) that are conveniently stuck together. In the simplest terms the function of these two pumps is to gather venous blood from the body and propel it to, and through, the lungs from which it is again gathered and propelled out toward and through the peripheral tissues. "All" of the blood in the body, approximately 5 liters, passes through this circuit in one minute.
It is notable that the segment of the circulation from the right ventricle through the lungs and back to the left atrium (Pulmonary Circulation) is a relatively short circuit. Due to the low resistance of the pulmonary vascular bed, flow of blood through the lungs can be driven by a small pressure difference. In contrast the circuit followed by blood exiting the left ventricle into the aorta, flowing through the peripheral tissues and returning to the right atrium (Systemic Circulation) can be quite lengthy. Total resistance to blood flow in this circuit is higher than in the pulmonary circuit. Therefore, pressure in the systemic arteries is significantly higher than in the pulmonary arteries and the left ventricle must generate a much higher pressure to expel blood into the systemic arteries and through the systemic circuit.
Although the left and right hearts function in a coordinated manner, the blood flows first through one side (e.g. right heart) and then through the other. It should be evident that in the long term, at least, the volume of blood exiting the right heart (Right Heart Cardiac Output) must be the same as the cardiac output of the left heart. Since the two sides of the heart contract in a coordinated manner, the number of beats per minute (Heart Rate) of the two sides must be the same and the volume of blood ejected from each side with each contraction (Stroke Volume) must be the same, on the average.
II. Sequence of events as blood passes through the heart
Since the major function of the heart is to propel blood, it is valuable to follow the pathway that blood follows as it passes through the heart. As blood passes through the heart landmarks and events will be evident that can be explored in detail later. It is useful to begin with blood flowing toward the right atrium from the superior vena cava and inferior vena cava. This blood is returning from the systemic circuit and it is draining out of the tissues (muscle, brain, gut, etc,). It has a relatively poor oxygen content, relatively high content of carbon dioxide. Pressure in the vena cavae is very low, perhaps only 1 mmHg. Approximately 5 liters of blood returns to the right atrium per minute under resting conditions in a healthy adult person. The blood that has collected in the right atrium flows into the right ventricle through the tricuspid valve when right ventricular pressure is lower than atrial pressure, effectively filling the right ventricle during cardiac diastole. During contraction of the right ventricle, blood is ejected from the ventricle through the open pulmonic valve into the pulmonary artery. Pressures in the pulmonary artery typically reach levels of 25 mmHg during peak contraction (systole) and fall to 10 mmHg between contractions (diastole).
Blood in the pulmonary artery flows through the pulmonary arterioles and pulmonary capillaries, discharges its excess carbon dioxide and replenishes its oxygen content, and flows back to the left atrium via pulmonary veins. Blood pressure in the left atrium is also very low, perhaps 0 to 1 mmHg. Blood accumulated in the left atrium flows through an open mitral valve and fills the left ventricle during diastole. During ventricular contraction, blood is ejected from the left heart through an open aortic valve into the aorta. The aorta is the initial and largest artery in the systemic circuit. Pressures in the aorta (120mmHg during systole and 80 mmHg during diastole) are significantly higher than pressures in the pulmonary circuit.
Typically the left ventricle of a healthy adult at rest contains 120 ml of blood when completely filled (End Diastolic Volume) and ejects perhaps 80 ml of blood during each systole (Stroke Volume), leaving behind 40 ml of blood at the end of systole (End Systolic Volume). The fraction of blood ejected during each heartbeat (Ejection Fraction) is calculated as the Stoke Volume divided by End Diastolic Volume. Each of these measured volumes are highly variable from individual to individual. They vary normally with exercise and other changes. They also may vary with abnormal changes in cardiac function. Thus knowledge of cardiac volumes, pressures, and ejection fraction is useful for identifying changes in cardiac function.
III. Structural Items of Note.
A. The atria primarily function to gather blood returning from the capillaries of the pulmonary and systemic circuits. They do not generate any significant pressure to propel blood into the ventricles, but the orifices of the tricuspid and mitral valves are large openings with very low resistance to flow. Thus the atrial walls are exceptionally thin, containing mainly connective tissue with a little cardiac muscle.
In contrast, the ventricles eject blood against a high pressure in the arteries. Therefore, although resistance to flow through the normal pulmonic and aortic valve openings is very low, the resistance through the remainder of the circuits is high, especially in the systemic circulation. Thus the ventricles generate much higher pressures than the atria and the thickness of the ventricular muscle wall is much greater than the atria. In addition, since the resistance of the systemic circuit is higher than that of the pulmonary circuit, the left ventricle is much thicker-walled than the right.
IV. Cardiac Valves

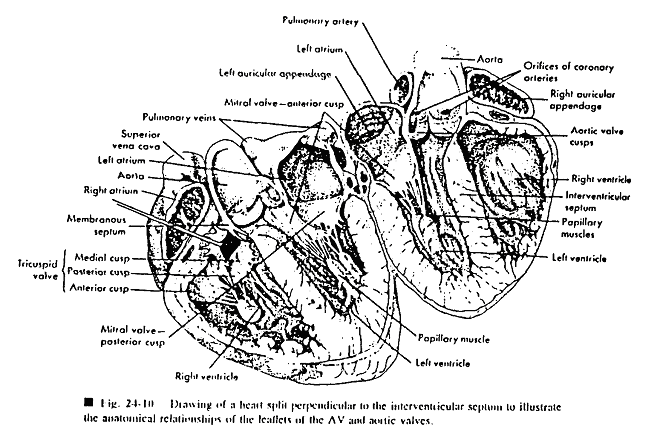
(Reprinted from Principles of Physiology 3rd ed., (1993) by R.M. Berne & M.N. Levy, Fig 24.11, page 406, with permission from Elsevier.)
A. Structure and Normal Function
The cardiac valves function to assure unidirectional flow of blood through the heart, from atria to ventricle, from ventricle to artery, and to prevent backflow. The valves are entirely passive tissues containing a tough, flexible fibrous core covered with endothelium. They contain no contractile muscle and move only because of the pressure changes on either side. These inert, passive characteristics make the replacement of valves a relatively simple process.
The Atrioventricular Valves (AV Valves) are the Tricuspid and Mitral Valves. The Tricuspid valve has three leaflets, or cusps, and separates the right atrium from the right ventricle. When blood pressure in the right atrium is higher than that in the ventricle, the tricuspid valve opens with cusps opening into the ventricle space, providing a large, low resistance venue for blood to flow and fill the ventricle. During systole, however, pressure increases in the ventricle and becomes higher than that in the atrium. The tricuspid cusps are pushed out of the ventricle until they meet, occluding the opening. Under normal conditions, the leaflets of the tricuspid valve are attached via the chordae tendinae to papillary muscles of the right ventricular wall. This attachment prevents the tricuspid from being blown back into the atrium during systole.
The Mitral valve separates the left atrium from left ventricle and functions in the same manner as the Tricuspid. The only difference between the two is that the mitral valve has only two valve cusps.
The Semilunar Valves are the Pulmonic and Aortic valves and they separate the Pulmonary artery and Aorta from their respective ventricles. They are named for the half-moon shape of each of their valve cusps. Both valves have three semi-lunar cusps. During systole, the high pressure in the ventricle pushes open the valve. During diastole, the ventricular pressure falls below that of the artery and the valves are pushed shut. The unique semi-lunar shape of the valves allows them to shut and occlude the opening without being tethered by chorda tendinae like the AV valves.
B. Abnormal Valves
Normally the cardiac valves are flexible and tough. When opened, they provide a large, low resistance orifice for flow. When closed, they close completely, preventing any backflow. However, under abnormal conditions the valve may become deformed or stiffened and not open completely (Stenosis). The narrowed orifice that results may reduce flow through the valve and reduce ventricular output and/or ventricular filling.
Similarly a valve may fail to close completely due to malformation or stiffening. Under such conditions the valve may allow back-flow from ventricle to atrium during systole or from artery back into ventricle during diastole. Such an incompetent valve, by allowing regurgitation, may also reduce effective cardiac function.
Calcification of a valve, one of the long-term consequences of rheumatic heart disease, may cause the valve to be both stenotic and incompetent at the same time.
V. Changes in ventricular pressure and volume during a single cardiac cycle.
The mechanical events of the cardiac cycle are also conveniently summarized by pressure-volume (PV) loops. These are plots of left ventricular pressure as a function of left ventricular volume.
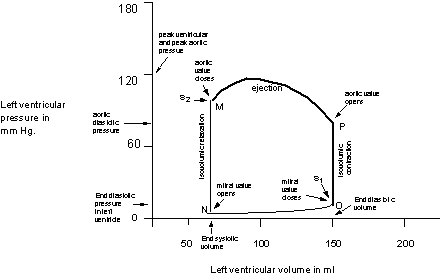
While the PV loop shown above does not contain the element of time, it nevertheless, is accomplished in one second at a heart rate of 60/minute. Thus the events of the cycle can be conveniently described in their normal sequence.
Ventricular systole is represented by the bold border of the loop, and ventricular diastole is represented by the non-bold border.
Ventricular filling: At point N, left ventricular pressure drops below left atrial pressure causing the mitral valve to open. Initially ventricular filling is rapid, but as ventricular pressure rises to that of the atrium filling slows, and final filling is accomplished by atrial contraction (Note that ventricular pressure is higher at point O than at N). The entire interval of filling is represented by segment N - O.
- End systolic volume (ESV) is the ventricular volume (70 ml) at point N.
- End diastolic volume (EDV) is the ventricular volume (150 ml) at point O.
Usually, EDP bears a direct relationship to EDV.
- EDV (150 ml) minus ESV (70 ml) = Stroke volume (SV = 80 ml)
- EDV (150 ml) also represents the entire ventricular volume at the end of ventricular diastole.
- SV (80 ml)/ EDV (150 ml) is the ejection fraction = 0.53
Ventricular depolarization, as indicated by the QRS complex of the EKG precedes ventricular contraction by about 50 msec.
The rapid rise in pressure (segment O-P on the graph) occurs because the contracting ventricle raises the ventricular pressure above atrial pressure causing the mitral valve to close. This along with closure of the tricuspid valve of the right ventricle creates the first heart sound, S1. The ventricle now contracts with all valves closed; thus ventricular volume remains constant giving rise to the descriptive term of isovolumic contraction for this brief (50-75 msec) phase.
When the ventricular pressure exceeds the aortic pressure (point P) , the aortic valve opens and ejection of blood occurs. At first ejection is rapid, but as peak systolic pressure is reached, ejection slows. The ejected blood distends the elastic walls of the aorta, but as ejection slows aortic pressure drops and the elastic arterial walls recoil. This momentarily reverses the flow of blood and closes the aortic valve (point M), thus ending the interval of ejection. Closure of the aortic valve (and the near simultaneous closure of the pulmonic valve of the right ventricle) creates S2.
At M all valves are again closed and the ventricle is relaxing at a constant volume (isovolumic relaxation). Ventricular pressure drops rapidly, until it falls below left atrial pressure again and a new cycle (new PV loop) begins.
Additional information in the PV loop:
- The aortic pressure at point P is aortic diastolic pressure, and the peak pressure during ejection is aortic systolic pressure. The pressure at point M is correlated with the aortic pressure recorded at the dicrotic notch.
- A Pressure-Volume loop for the right ventricle has a similar shape to that of the left ventricle. EDV is very similar for the left and right ventricles, as is SV. However, pressures reached during isovolumic contraction (and during ejection) are considerably lower in the right ventricle.
The shape of the PV loop changes with increased or decreased filling (preload) of the ventricle, with increased or decreased aortic pressure (afterload), and with increased or decreased cardiac contractility. Examples of conditions in which these factors change are given in the study questions.
I. Events of the cardiac cycle:
The pumping action of the heart can best be understood if the major electrical and mechanical events of one cardiac cycle are related in a single figure. This figure is based on data from a dog, thus the ventricular volume and aortic blood flow are considerably less than that of an adult human. A right ventricular pressure curve (not shown) would be similar to the left ventricular pressure curve, but with lower pressures. The description of the cardiac cycle that follows the figure presents the events of the cycle sequentially.

A. Electrical activation:
Electrical activation of the heart begins with depolarization of the SA node which initiates a wave of depolarization that spreads along and down the atrial muscle creating the P wave on the EKG (see bottom of figure 24.13). The wave of depolarization is briefly delayed as it reaches the right posterior portion of the inter-atrial septum, i.e., the AV node. Next, the depolarization spreads through specialized conduction pathways, i.e., the bundle of His, the bundle branches, and the Purkinje fibers. Subsequent depolarization and repolarization of the ventricular muscle is reflected in the QRS complex and the T wave of the EKG, respectively. Because these electrical events are recorded by EKG electrodes almost instantly, and because EKG can be recorded non-invasively, events of the EKG can serve as approximate time-markers for other events of the cardiac cycle.
B. Atrial contraction
Atrial contraction (which precedes ventricular contraction by about 0.1 sec.) adds little blood to the ventricular volume except during exercise. As is explained in D below, most of the blood enters the ventricles during the first third of diastole fast filling phase).
C. Ventricular contraction:
Contraction of the ventricular muscle raises the pressure in the ventricle (making ventricular pressure greater than the atrial pressure); thereby causing the AV valves [tricuspid between right ventricle and right atrium; bicuspid (mitral) between the left ventricle and left atrium] to close. The AV valves close due to the pressure gradient, but are prevented from bulging excessively into the atria by the chordae tendinae.
(Note: surfaces of heart valves and the interior surface of the heart are lined by a single layer of endothelial cells called ”endocardium”. Epicardium is the outermost layer of the heart and is identical to the visceral pericardium that is the inner serosal layer of the pericardium.)
Following closure of the AV valves (and as ventricular contraction proceeds), the pressure in the ventricles rises rapidly (only left ventricular pressure is shown in fig 24.13), because the semilunar valves (pulmonic for the right ventricle, and aortic for the left) are still closed. Moreover, the volume of the ventricles remains constant; hence this interval of rapidly rising ventricular pressure is called the interval of isovolumic contraction.
As contraction proceeds, the pressure in the ventricles reaches a point where it exceeds the pressure in the aorta (left ventricle) and pulmonary artery (right ventricle). This pressure gradient opens the semilunar valves and blood is rapidly ejected. Pressure in the aorta (and pulmonary artery) reaches a peak (peak systolic pressure) and then begins to fall. Ejection of blood continues until the pressure in the aorta (left side) and pulmonary artery (right side) exceeds that of their respective ventricle. At this point the semilunar valves close and ejection ceases.
During ventricular contraction, the rapid ejection of blood distends (stretches) the arteries. As ejection slows, the elastic recoil of the arteries propels blood not only distally, but proximally as well, the latter helping to close the semilunar valves. The pressure wave created from the recoil of blood striking the closed semilunar valve creates the dicrotic notch in a recording of the aortic pressure. The dicrotic notch marks the end of ventricular systole and the beginning of diastole. It also coincides with the second heart sound, and the beginning of the interval of isovolumic relaxation.
D. Ventricular filling:
Ventricular pressure drops rapidly during isovolumic relaxation, and when ventricular pressure descends to less than atrial pressure, the AV valves open and blood flows from the atria into the relaxed ventricles. Because normal AV valves have large openings, they offer little resistance to flow; so even the small pressure gradient between the atria and the ventricles causes the ventricles to fill rapidly. As the ventricles fill the ventricular walls stretch, ventricular pressure rises and filling slows. The final filling of the ventricles is accomplished by atrial contractions as described in B above.
E. Other characteristics of the cardiac cycle:
- 1. Atrial Pressures
As compared to ventricular pressures, atrial pressures are low. Contraction of the atrium increases atrial pressure slightly, and creates the "a" wave of the atrial pressure recording. During isovolumic contraction of the ventricle, the A-V valves bulges into the atrium, thus raising atrial pressure for a second time, and creating the "c" wave. Pressure in the atrium then drops slightly during rapid ventricular ejection, because the entire ring of AV valves descends as the ventricle rapidly ejects blood. This action gives the atrium a greater capacity, thus atrial pressure falls. Next, during reduced ventricular ejection and isovolumic relaxation, blood fills the now relaxed atrium causing the atrial pressure to rise for a third time, i.e. producing the "v" wave. Atrial pressure falls when the AV valves open and the blood flows into the ventricle.
- 2. Venous Pressures
The pressure waves of the right atrium reflect to the large systemic veins, (e.g. the jugular vein) thus a recording of jugular venous pressure also displays "a", "c", and "v" waves. Pressure waves in the atria and large thoracic veins (vena cavae) are superimposed on pressure changes produced by the respiratory cycle, i.e., pressure decreases during inspiration and increases during expiration.
- 3. Cycle Duration
At resting heart rates (< 75 beats/min), each cardiac cycle lasts about 800 msec (0.8 sec). Ventricular diastole (550 msec) lasts almost twice as long as ventricular systole (250 msec). At rapid heart rates, both systole and diastole shorten, but diastole shortens much more than systole.