Arterial and Venous Systems (Chapter 21)
Objectives:
- Explain how the pulsatile blood flow in the large arteries is converted into an almost steady flow in the capillaries
- Explain the factors that determine the systolic and diastolic arterial pressures and the arterial pulse pressure
- Describe the common procedure for measuring the arterial blood pressure in humans
The Arterial System
- The arterial system serves to conduct blood from the heart to the tissues, and to dampen pulsatile flow thereby creating near-continuous flow at the tissue level. With each cardiac systole, the volume of blood in the arterial system increases causing arterial pressure to rise. At the distal end blood flows continuously into capillaries thereby reducing arterial volume and pressure during diastole. As a result the arterial pressure oscillates through cycles - systolic (high) and diastolic (low).

(Reprinted from Principles of Physiology 3rd ed.,(2000) by R.M.Berne & M.N.Levy, page 238 with permission from Elsevier.)
- Large arteries are compliant: Larger arteries expand to absorb a significant fraction of the stroke volume, say 80%. These compliant vessels swell during systole. During diastole the elastic recoil (the opposite of compliance) maintains sufficient blood pressure to provide uninterrupted flow to the capillary beds (Fig. 1).
- Mean arterial pressure: If arterial pressures are recorded as a function of time, a pattern similar to that shown in Fig. 2 is obtained. Arterial pressure reaches a peak (systolic pressure) and then declines (diastolic pressure) until the next systole. The minimum arterial pressure occurs just before systole (arterial diastolic pressure). The difference between the systolic and diastolic pressures (systolicdiastolic) is the pulse pressure. The average arterial pressure is between the systolic and diastolic pressures. Mean arterial pressure (MAP) is represented by the area under the curve integrated over the cardiac cycle. The mean arterial pressure can be approximated by adding 1/3 of the pulse pressure to the diastolic pressure.

As the heart beats faster the MAP will rise because the heart spends more time in systole and less in diastole. As arterial pressure falls after systole, a notch in the pressure wave appears in the aorta and proximal arteries. The dicrotic notch represents the pressure variations occurring at the time of closure of the aortic (semi-lunar) valve. From the time of the dicrotic notch until the aortic valve opens during a subsequent systole, pressures in the artery and left ventricle diverge; left ventricular diastolic pressure falls to near zero.

- Relationship of arterial blood flow and arterial pressure: The velocity of blood flow in the ascending aorta has been recorded simultaneously with aortic pressure (Fig. 3). It is evident that the greatest rate of flow occurs early in systole with blood flow declining considerably by the end of systole. In fact as the left ventricle relaxes and ventricular pressure falls below aortic pressure the blood flow in the ascending aorta may momentarily reverse direction.
- Effect of compliance on pulse pressure: Each stroke volume (SV) that is pumped by the left ventricle joins the blood already in the aorta and its larger branches. During systole, about 20% of this added volume flows (“runs off”) to smaller more peripheral vessels, while the remainder swells the aorta. During diastole, the driving force for continued flow of blood to the tissues is the elastic recoil of the distended aorta and large vessels. The compliance (dV/dP) of blood vessels is inversely related to their elastic recoil, i.e., rigid vessels have low compliance. Generally, the compliance of the arteries diminishes with age (Fig. 4). The result is a larger pulse pressure (higher systolic, lower diastolic) for a given stroke volume. In extreme cases, the pulse pressure can become large and the pulse feels like a “water hammer pulse”. The resulting increase in cardiac afterload (systolic pressure) increases the required work of the heart. A change in arterial compliance does not change mean arterial pressure, only pulse pressure.
- Interaction of peripheral resistance, stroke volume, and compliance on the determination of arterial pressure: Mean arterial pressure is directly proportional to cardiac output (CO) and total peripheral resistance (TPR). A 50% increase in cardiac output whether by increased SV or heart rate (or both) will increase mean arterial pressure by 50% - provided that total peripheral resistance remains constant.

(Reprinted from Principles of Physiology 3rd ed., (2000) by R.M. Berne & M.N. Levy, page 238 with permission from Elseview.)

The compliance (C) of the arteries is equal to the added volume, i.e. stroke volume (SV), divided by the pulse pressure (AP) the added volume produces. Stated in formula:
The pulse pressure (AP) is directly proportional to the SV and inversely proportional to C.
If the size of the SV increases, thereby increasing systolic pressure, diastolic pressure will also be increased (provided that TPR and heart rate (HR) remain constant): the volume added to the arteries does not “run off” quickly enough to allow diastolic arterial pressure to return to its value before the volume is added.
Systolic pressure is a function of stroke volume and arterial compliance. A decrease in C (unaccompanied by any change in SV or TPR) increases systolic pressure but decreases diastolic pressure. As a result pulse pressure increases, but mean pressure is unchanged.
Diastolic pressure is a function of total peripheral resistance, arterial compliance, systolic pressure, and the time between beats.
- Changes in diastolic, and pulse pressures in chronic hypertension: Patients with chronic hypertension (elevated MAP) may have elevated systolic, diastolic, pulse pressures. Diastolic pressure may be 10 - 40 mmHg above the normal of 80 mmHg and systolic pressure may be 50 - 150 mmHg above the normal of 120 mmHg. Sometimes pulse pressure may be within the normal range. Increased MAP is a function of TPR and CO, not arterial compliance.
- Changes in arterial pressures with age: In the American population average blood pressure increases with age beginning around 20 years of age. The same phenomenon is not seen in all societies. It is not clear whether the increase in blood pressure with age is 'normal' and unavoidable or simply 'common' and avoidable.
- Characteristics of the arterial pressure pulse wave: The sudden stretch of the ascending aorta produced by the ejected SV sets up a vibration wave that travels along the aorta and the arterial branches. This vibration wave travels considerably faster along the arterial wall than the ejected blood (4000-6000 cm/sec for the vibration wave compared with 20-40 cm/sec for blood flow) The vibration wave is the “palpable pulse” that one feels in peripheral arteries. The palpable pressure-pulse is conducted faster in non-compliant (stiff) arteries than in compliant arteries.

The arterial pressure recorded from a catheter within the artery changes in character depending on the location of the catheter (Fig. 6). Generally, with further distance from the ascending aorta, the systolic portion of the pressure wave narrows and increases in amplitude. Nevertheless, mean arterial pressure decreases. (It must or blood would not flow from the heart to the capillaries.) These changes are related to the decreasing diameter and decreasing compliance of arteries with distance from the heart. Both changes increase the amplitude but decrease the duration of the pressure wave.
Measurement of blood pressure in humans:
- Direct measurement: In patients who need constant blood pressure monitoring, catheters are placed in an artery allowing arterial pressure to be measured directly (see Fig. 6)

- Indirect measurement: An inflatable bag (cuff) connected to a manometer (sphygmomanometer) is used to occlude the flow of blood completely in an arm or leg. If the bell of a stethoscope is placed over a major artery just distal to the occluded artery, no sound will be heard as no flow is going through the artery. As pressure is slowly decreased in the cuff, at some point blood will begin to spurt through the occluded artery - but only during systole. As the blood spurts through and impacts the collapsed distal portion of the artery, faint tapping sounds are heard through the stethoscope. The pressure at which sounds are first heard corresponds to systolic blood pressure. As the pressure in the cuff is decreased further, the sounds become progressively louder, then muffle and finally disappear. Their disappearance corresponds approximately to diastolic pressure, because at this pressure, blood flows through the artery unimpeded and without turbulence during diastole as well as systole.
For accurate recording, the sphygmomanometer should be positioned at the same level as the heart so that hydrostatic pressure (gravity effect) neither adds nor subtracts from the actual blood pressure (Fig. 8). Blood pressure should be routinely measured in both arms to assure that no unique circumstances in one arm are disturbing the results.
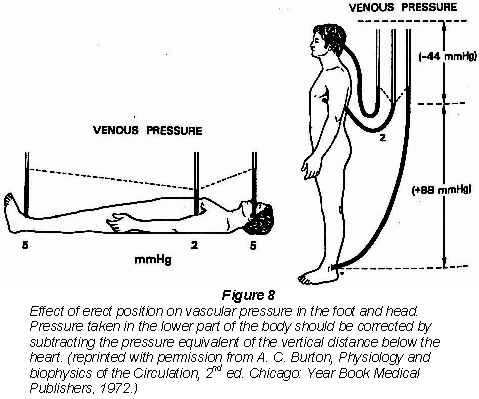
Blood pressure recorded from an arm (at the level of the heart) may be lower when the patient is standing than when seated or lying down. Postural hypotension represents the situation observed when blood pools in the lower limb veins on standing.
Blood is returned from the extremities through veins with valves that only allow blood to flow in the direction of the heart. As muscles contract the veins are compressed and the return of blood is directed toward the heart. Four valves can be seen within the circle.
